One look at Aedes aegypti gives an immediate impression of its menacing nature. The telltale dark and white bands on the mosquito’s legs and other body parts bring a sense of foreboding and hardship. Sleek, silent, and stealthy, Ae. aegypti is the primary vector for several important, debilitating, and sometimes fatal human diseases including dengue, Zika virus, yellow fever, and chikungunya. The species is cause for mounting concern on many levels, as its biology, behavior, and ability to adapt have made Aedes aegypti one of the most pervasive and daunting public health challenges in the modern world.
Biology and Life Cycle
The first mosquito ever associated with the spread of disease, Ae. aegypti is also the most studied of all mosquito species.1 From its humble beginnings in the African wild to a footprint that spans the globe, this durable and opportunistic insect has become a formidable opponent of vector control efforts worldwide.
To fully appreciate the threat of Aedes aegypti, one should begin with its biology. While the Aedes genus comprises over 700 species, Ae. aegypti has several distinguishing features that contribute to its success. Like all mosquitoes, the life cycle of Ae. aegypti includes four distinct stages: egg, larva, pupa, and adult. But unlike many other mosquito species – which lay their eggs in floating rafts – Ae. aegypti lay their eggs individually. One female can lay up to 100 to 200 eggs per batch, and up to 1,000 eggs during her lifetime. These eggs are especially tough and can persist over several months waiting for optimal conditions for hatching. They can tolerate a wide range of temperatures, enabling them to survive in both tropical and temperate regions. They can withstand extreme heat and cold.
Ae. aegypti eggs also possess adhesive properties, enabling them to attach to various surfaces such as the walls of water containers, tree holes, or even plants near water sources. This adaptation helps prevent the eggs from being washed away by rain or other water disturbances, ensuring their survival. Their hard outer shell also provides protection against predators such as aquatic insects, fish, and other organisms that might consume the eggs, increasing their chances of successfully hatching and developing into larvae.

Fedaro/Wikimedia Commons
The Ae. aegypti life cycle is completely dependent on access to standing water, which is why Ae. aegypti mosquitoes are often found near humans. Small amounts of water can collect in things like buckets, bowls, animal dishes, discarded tires and other refuse – all of which are prime breeding grounds for Ae. aegypti.
Once conditions are right (typically when they become submerged in water), Ae. aegypti eggs hatch into larvae within about 48 hours. During four subsequent instar stages, the larvae feed on organic matter in the water and molt several times, growing larger with each molt. The larval stage lasts about five to seven days under optimal conditions. After the fourth larval instar, the mosquito enters the non-feeding pupal stage (two to three days) where it undergoes metamorphosis into its adult form. Depending on environmental conditions and other risk factors such as access to food and exposure to pesticides or predators, adults can live from a few weeks to a month or more.
Adult male Ae. aegypti are content to feed on nectar and other sugars, while females also feed on blood. Blood provides the protein necessary for egg production and serves as the vehicle through which the mosquito transmits disease. When a female Ae. aegypti mosquito bites a person infected with a vector-borne diseases, it ingests the virus along with the bloodmeal. After an incubation period within the mosquito, the virus can then be transmitted to the next person the mosquito bites.
Distribution and Disease Transmission
Beyond its physical characteristics, unique aspects of Aedes aegypti’s behavior also differentiate it and contribute to its success. Since Ae. aegypti prefer breed near humans, its spread is closely linked to human movement as well.
It is widely accepted that Ae. aegypti began as a forest subspecies in its native Africa, then followed humans as agriculture developed. During the 15th to the 19th century, Ae. aegypti migrated to the Americas and Europe on ships in the African slave trade.2 Today, Ae. aegypti is found in nearly all tropical, subtropical, and even in some temperate climates.
In the Americas, Ae. aegypti can be found from the Southern U.S. (primarily in the Southeast, the Gulf Coast, and parts of Arizona and California) and southward to Argentina. It remains entrenched across sub-Saharan Africa, as well as in parts of North Africa. Ae. aegypti is widespread in Asia and can be found in many countries including India, Thailand, Vietnam, the Philippines, and Malaysia. It inhabits parts of the Middle East, northern Queensland in Australia, and is present on many Pacific and Indian Ocean islands including Hawaii, the Caribbean, the Maldives and Seychelles.
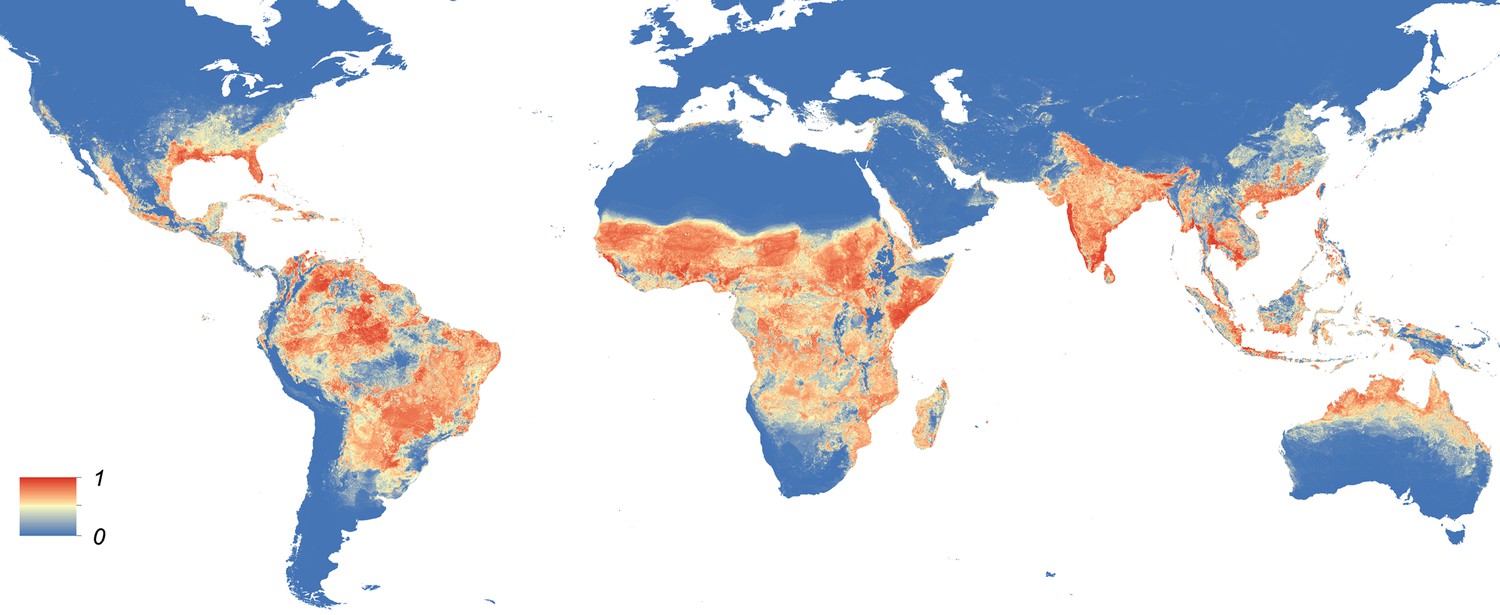
https://doi.org/10.7554/eLife.08347.004
Climate change and urbanization combined with the mosquitoes’ adaptability, and increasing global travel and trade are all contributing to an ever-expanding distribution of Aedes aegypti. Travelers who get infected while in one region can then be bitten by Ae. aegypti mosquitoes after they return home, introducing the virus to local mosquito populations.
Climate change has become a particularly important factor in recent years. As temperatures rise and rainfall patterns change, the areas that are suitable for Ae. aegypti are also changing. Warmer temperatures can accelerate the mosquito’s development, reproduction rates, and the viral replication within the mosquito, leading to increased transmission risk. The ability of Ae. aegypti eggs to withstand desiccation and extreme temperatures in the face of changing climate also allows them to survive in harsh conditions for several months, giving them a high survival rate.
The actual distribution of Ae. aegypti may be more extensive than what is currently documented due to underreporting or lack of surveillance in some areas, and it is important to understand that the distribution of Ae. aegypti is not static. In addition to the factors already mentioned, control efforts can also influence their geographical range. Good examples of the impact of human intervention include concerted Ae. aegypti eradication efforts that took place in Brazil and the U.S. in the mid-1990s. While these programs were initially successful, control efforts eventually waned. The result in both cases was that Ae. aegypti was back, in force, by the turn of the century.3
In addition to their preference for container breeding, the feeding habits of Ae. aegypti contribute to its success. Since Ae. aegypti is a day-biting mosquito, many of the control measures used against night-biting mosquitoes – such as Insecticide-Treated Nets and Indoor Residual Sprays – are less effective against Ae. aegypti. This translates into opportunities for disease transmission.
The Many Impacts of Aedes aegypti
The cumulative impact of Ae. aegypti is expansive and extremely challenging to measure, in part because that impact can take so many forms.
From an economic standpoint a recent study conducted by researchers in France estimates the total raw costs (damage, losses, and management) for dengue, Zika and chikungunya between 1975 and 2020 exceeded a staggering $87 billion (see table).4 Another study conducted by researchers in the U.S. estimated the total combined costs for dengue alone to be around $8.9 billion.5 From a regional incidence perspective, a 2013 study led by researchers at Oxford University estimated that Asia bore the burden of 70% of all dengue infections globally in 2010.6 These are just a few examples of the toll Ae. aegypti wages on society.
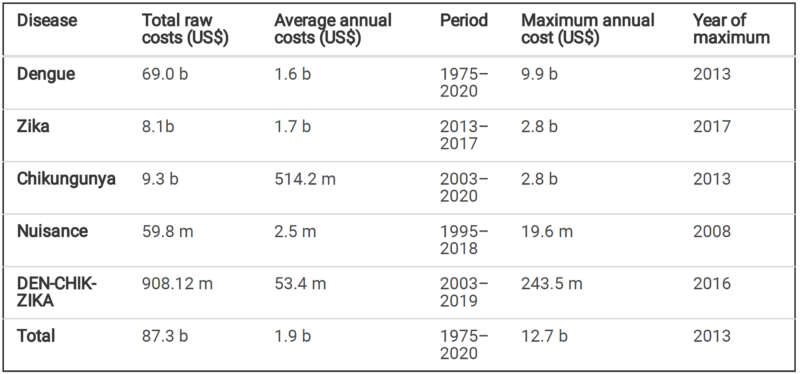
Roiz et al.
Whatever form the impact takes, that burden falls disproportionately on poorer countries and communities where healthcare resources are limited, vector control programs may be inadequate, and people have fewer resources to prevent and treat illness. Conditions in these communities often favor mosquito breeding as well. A lack of reliable access to clean water, for example, creates the need for water storage in open containers.
Still other vulnerable populations include children and pregnant women. Children are known to be especially susceptible to severe dengue fever (dengue hemorrhagic fever), which can cause bleeding, blood plasma leakage, and low platelet count, and can ultimately be life-threatening. It is also thought that children may be fundamentally more exposed to mosquito bites due to their activities and the locations where they play and learn.
According to the CDC, a pregnant woman already infected with dengue can pass the virus to her fetus during pregnancy or around the time of birth. This can have harmful effects including death of the fetus, low birth weight, and premature birth.7 The most significant concern for pregnant women pertaining to Ae. aegypti is likely the Zika virus, which can also be transmitted from a pregnant woman to her fetus. As the world witnessed during the 2015/2016 Zika outbreak, Zika virus infection during pregnancy can cause pronounced birth defects, including microcephaly (a condition where a baby’s head is much smaller than expected due to abnormal brain development) and other severe brain anomalies. These can lead to long-term developmental problems in the child.
While Ae. aegypti transmitted diseases like dengue, Zika, and chikungunya all have the capacity to lead to chronic physical health issues, evidence suggests these conditions are often associated with mental health problems as well. Depression and anxiety, due to the stress and challenges of managing long-term illness, are good examples. There can also be stigma associated with and fear of infection, which can lead to social isolation, as well as economic and psychological impacts, among the afflicted.
The US Centers for Disease Control and Prevention (CDC) estimates that more than 400 million people are infected by dengue each year.
As we saw during the COVID-19 pandemic, disease outbreaks can put a tremendous strain on healthcare workers. The stress, long working hours, and emotional toll of dealing with severely ill patients can lead to burnout and other mental health issues. These examples highlight an often-ignored dimension of the burden of diseases transmitted by Ae. aegypti.
Controlling Aedes aegypti
Controlling the diseases that Ae. aegypti spread begins with controlling the vector. There are many approaches to accomplishing this, but none is a silver bullet. As with any species of mosquito, successful control of Ae. aegypti requires an integrated approach that employs a range of well-planned strategies, interventions, and technologies that meet the needs of the situation.
Since Ae. aegypti prefer containers, any effective control program involves eliminating potential breeding sites. Removing potential breeding containers (tires, flowerpots, buckets, etc.), routinely dumping them, or ensuring they don’t collect water can dramatically reduce mosquito populations. While this approach is not new, the sophistication and reach of public health education campaigns have greatly improved with the advent of modern communication technologies. Some of the most successful control campaigns include educational components with a focus on informing communities about the behaviors of Ae. aegypti and what actions individuals can take to reduce populations.
The use of chemical insecticides, bioinsecticides and other biological controls also play a pivotal role. Personal protective measures like wearing long-sleeved clothing and using insect repellent are the simplest of these interventions.
Chemical adulticides kill adult mosquitoes and chemical larvicides kill mosquito larvae in breeding sites. But the overuse of chemical insecticides over the past many decades has led to widespread resistance in mosquito populations, making this approach less and less effective over time. Insecticide resistance if often cited as one of the biggest threats to global public health (see Resistance in the Limelight, Public Health Landscape, February 2023).
One form of biological control involves introducing natural predators of mosquitoes, such as certain species of fish or copepods, into breeding sites to reduce mosquito populations. This method is typically more environmentally friendly than chemical control but can be less effective in urban areas where breeding sites may be small and dispersed. Another important alternative to chemicals is biological larvicides – substances derived from naturally occurring microorganisms that can be highly selective and affect only mosquitoes and closely related organisms.
The most commonly used biological larvicide is the bacterium Bacillus thuringiensis israelensis, or Bti. As part of its natural ecology, Bti produces toxins that are harmful to mosquito larvae but safe for most other organisms, making it an environmentally friendly alternative to chemical controls. Furthermore, Bti has multiple modes of action, which makes it an important tool for vector control managers, as resistance to it has never been observed in the field.

Ground-based applications have been a reliable way to deliver Bti into the small and difficult-to-access (cryptic) habitats where Ae. aegypti breed, and pioneering research surrounding wide area applications of Bti began in Southeast Asia in the early 2000s. In 2010, the first aerial application of Bti was used in the Florida Keys to stem the state’s first dengue outbreak in 75 years. Aerial application of Bti was also used effectively to break the Zika transmission cycle in Miami-Dade County in 2016.
Additional innovations in Ae. aegypti control are in the study phase. The “sterile insect technique” involves releasing male mosquitoes that have been sterilized with radiation into the environment. These males mate with wild females, but no offspring are produced, reducing the mosquito population over time. Another method involves genetically modifying mosquitoes to carry a gene that prevents their offspring from reaching adulthood. Yet another modern approach involves infecting Ae. aegypti mosquitoes with Wolbachia, a type of bacteria that naturally occurs in many insect species but not typically in Ae. aegypti. The bacteria compete with viruses like dengue, Zika, chikungunya and yellow fever within the mosquito, reducing its ability to transmit diseases.
Factors that will influence large scale adoption of these techniques include the results of ongoing and future research, regulatory decisions, public acceptance, and the availability of funding for these methods.
Significant Challenges to Controlling Aedes aegypti
Urbanization and globalization continue to facilitate the spread of Ae. aegypti and the diseases it transmits. High-density urban areas provide ideal conditions for this mosquito, and global travel can rapidly transport the mosquito and its associated viruses to new areas.
Climate change is expected to increase the geographical range of Ae. aegypti and prolong mosquito breeding seasons, potentially leading to increased disease transmission.
Resistance to chemical insecticides remains a significant challenge because the cost of chemicals is relatively low. As a result of overdependence and overuse, many Ae. aegypti populations have developed resistance to these insecticides, making control efforts less effective.
Adequate funding and resources are crucial for implementing comprehensive and sustained control efforts, particularly in low-income countries that are heavily affected by diseases transmitted by Aedes aegypti.
Joining Forces Against Aedes aegypti
Given the significant impact of Aedes aegypti, several international initiatives and organizations are focused on combating these diseases, providing strategic guidance, technical support, and resources.
World Health Organization (WHO): The WHO has several initiatives focused on controlling Ae. aegypti including the Global Vector Control Response and the Global Dengue and Aedes-transmitted Diseases Consortium. These initiatives aim to strengthen countries’ ability to prevent, detect and respond to vector-borne diseases through strategic guidance and technical support.
Pan American Health Organization (PAHO): PAHO plays a major role in controlling Ae. aegypti and the diseases it vectors in the Americas. PAHO initiatives include training and guidance on vector control, surveillance, and outbreak response; research into new control methods; and public education campaigns.
Innovative Vector Control Consortium (IVCC): The IVCC partners with public, private, and academic sectors to develop and implement new and improved vector control tools and strategies. While the IVCC’s initial focus was on malaria, their work has since expanded to include other vector-borne diseases, including those transmitted by Aedes aegypti.
Bill and Melinda Gates Foundation: The Gates Foundation invests heavily in efforts to combat vector-borne diseases, including dengue and Zika. This includes funding for research into new control methods, vaccines, and diagnostics, as well as initiatives to strengthen health systems and improve disease surveillance.
World Mosquito Program (WMP): The WMP is a global not-for-profit initiative that works with communities around the world to prevent mosquito-borne diseases including dengue, Zika, chikungunya, and yellow fever.
What the Future Holds
The outlook for Ae. aegypti control is cautiously optimistic as we continue to make progress in several key areas, but control of this vector remains a complex and evolving challenge that requires ongoing research, multi-sectoral collaboration, and sustainable funding.
Adaptability and a long-term, integrated approach are key to success.
Along with new tools and strategies, the impact of diseases transmitted by Ae. aegypti has led to increased global collaboration and commitment to finding solutions. There is also a growing emphasis on community-based approaches to Ae. aegypti control, recognizing that public participation and behavior change are key components of successful control programs. While the future may be uncertain, there is little doubt that efficient and effective control of Ae. aegypti is a top priority in public health.
By Rick Melnick
*References can be found here.
