world health organization
Sand Flies: The Silent Biters Spreading A Deadly Disease
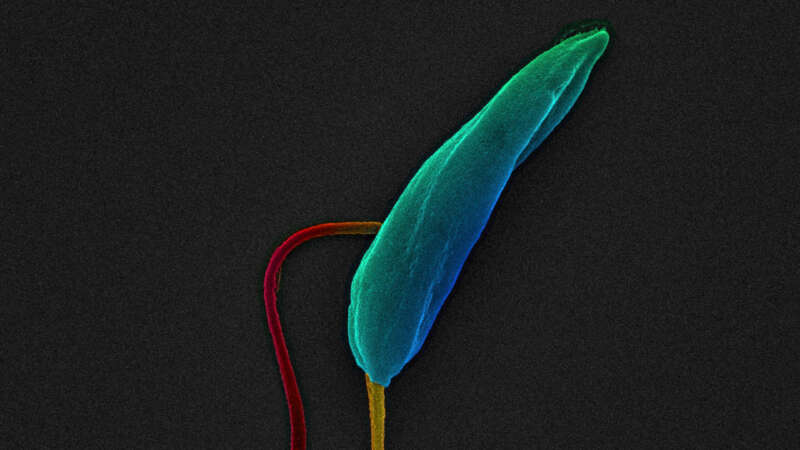
Phlebotomine sand flies are notorious biters. They not only cause great irritation but are also capable of spreading a deadly disease – visceral leishmaniasis.
While the World Health Organization states that currently 1 billion people live in areas endemic for leishmaniasis and at risk of contracting the disease, a recent study using a statistical model, predicted that visceral leishmaniasis (VL) is undergoing geographic expansion and 5.3 billion people could be at risk of acquiring the disease in the future.
Leishmaniasis currently occurs in approximately 90 countries. These countries are located in the warmer climates where sand flies thrive: in the tropics, subtropics, and in Southern Europe. Climate change and other variations in the environment have the potential to expand the geographical range of where sand flies can live and therefore where the disease can infiltrate the human population.
AI in Telehealth: The New Game Changers
AI transforms health-seeking from an ordeal to a convenience for a busy city-dweller and a boon for those with mobility issues or living in remote areas. A few taps of a finger can schedule a consultation, and visiting a physician becomes as effortless as sitting before a TV. Around 75% of healthcare organizations have found that integrating AI into their operations improved their ability to treat diseases effectively while reducing staff burnout.
Since physical examinations contribute to only 11% of the diagnostic process, with the patient’s history making up 76%, AI has become a valuable tool for helping medical professionals assess and interpret patient data more efficiently. AI algorithms can rapidly process large datasets, allowing medical professionals to identify potential health risks early – often before they are detectable by traditional methods.
Telehealth and telemedicine is a booming market, projected to grow at a compound annual growth rate of 23.2% between 2023 and 2028 as technology advances, regulations evolve, and patients and healthcare professionals accept telemedicine as a safe, economical and viable choice. AI is dramatically re-drawing the telehealth landscape in the areas of prediction, diagnosis, treatment and monitoring of diseases like heart disease, cancer, respiratory disorders and diabetes, which account for nearly 75% of deaths worldwide each year.
The Age of Firestorms
Dr. Roslyn Prinsley never imagined that stepping outside her home in Canberra would feel like walking into a smoke-filled abyss. But during Australia’s devastating bushfire season in 2019-2020, even in places untouched by flames, the air was so thick with smoke that breathing felt impossible.
“I asked myself, what are we doing here in the 21st century? We can’t actually go outside and breathe fresh air in one of the cleanest countries in the world,” she remembers thinking. “We can’t let this keep going.”
Dr. Roslyn Prinsley is the Head of Disaster Solutions at the Australian National University’s Institute for Climate, Energy & Disaster Solutions (ICEDS). Finding innovative ways to fight wildfires is part of her daily work – a task that has become more urgent than ever as wildfires grow increasingly frequent in Australia and across the globe due to climate change.
Wildfires are projected to rise 30% by the end of 2050, according to a report by the UN Environment Programme (UNEP) and its partner GRID-Arendal.
One of the recent wildfires in California became the most destructive in Los Angeles history, killing at least 29 people—a number expected to rise—and reducing over 10,000 homes to ash. A perfect set of environmental factors such as long-term drought, preceding heavy rainfall, and hurricane-force Santa Ana winds combined at the worst possible moment.
All of this turned the regular wildfire into what’s called a firestorm.
A Shining New Age of Vaccines
With vaccines, history repeats itself like music stuck in a loop. On the one hand, advancing technologies create vaccines against a growing list of lethal diseases and conditions. On the other hand, outrageous myths and conspiracy theories compete against science. Familiar and strong emotions run the gamut, from relief when deadly diseases like smallpox are eradicated to anger about perceived dangers to health, governmental overreach and threats to freedom of choice. While religious, commercial, pseudo-scientific and political interests cash in on the confusion, context and meaning are sometimes lost or forgotten. Telling facts apart from misinformation becomes difficult.
Understanding how vaccines are evolving can help better understand both why they are one of medical science’s supreme triumphs and also why the anti-vaccine movement continues to grow and influence so many.
Tick-ing Time Bomb: The Expanding Threat of Tick-Borne Diseases
Urbanization, resistance to pesticides, and, most critically, climate change are creating ideal conditions for global tick proliferation. As these 8-legged bloodsuckers expand their territories, the world should expect a corresponding rise in Lyme disease, spotted fever, Crimean-Congo hemorrhagic fever, tick-borne encephalitis, and other conditions that infect humans, pets, and livestock.
“This is an epidemic in slow motion,” a Centers for Disease Control (CDC) tick expert and research, biologist told the Associated Press.
Ticks live on every continent except Antarctica, and while estimates of annual tick populations vary, the scientific community agrees that their numbers are growing. Researchers also are unanimous that arachnids pose an increasing health risk as mild winters and longer summers associated with global warming kill off fewer individuals, give them longer to develop and feed, and make higher elevations and northerly latitudes that previously were too intemperate or elevated more hospitable.
Role of Social Determinants in Maternal and Child Health
About 287,000 women died during and following pregnancy and childbirth in 2020. Around 95% of these maternal deaths occurred in low and lower middle-income countries and nearly every death was preventable. Equally, children under the age of five continue to face differing chances of survival based on where they are born and raised.
A child born in sub-Saharan Africa is 11 times more likely to die in the first month of life than one born in the region of Australia and New Zealand, and a 15-year-old girl in sub-Saharan Africa is 400 times more likely to die in her lifetime due to issues related to childbirth than a 15-year-old girl living in Australia and New Zealand (with the ratio for SSA being 1 in 40, compared to ANZ being 1 in 16,000 women).
Shrinking Forests, Emerging Diseases
Dona Dora’s man is away from home a lot more these days. It didn’t used to be like that.
He leaves early, sometimes on foot, but increasingly on his bicycle, and heads into the forests surrounding Belém, the capital of Brazil’s Para province. He keeps his eyes open especially for five medicinal plants that are always in demand — sucuúba (Himatanthus sucuuba), copaíba (Copaifera spp.), andiroba (Carapa guianensis), barbatimão (Stryphnodendron spp.) and pãu d’arco (Tabebuia avellanedae).
Fifteen years earlier, he would have found all five within hours and been back for lunch, but times have changed. These days, medicinal forest plants in high demand are becoming harder to find as forests that have stood strong for millennia are cleared to make way for grazing pastures for millions of cattle, agriculture, and development.
Now, Dona Dora’s man can spend a whole day and not find more than a few plants. It might be late at night before he gets back home.
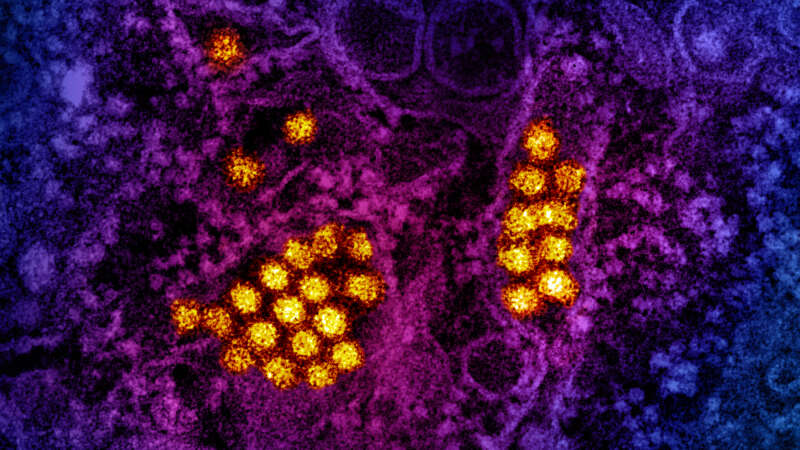
The Rise of Dengue: A Global Perspective
Around the world, dengue is considered the most common viral disease transmitted by mosquitoes that affects people. According to the World Health Organization (WHO), the disease is now endemic in more than 100 countries. In the first three months of 2024, over five million dengue cases and over 2000 dengue-related deaths were reported globally. The figures so far project that 2024 could be even worse than 2023, with the regions most seriously affected being the Americas, South-East Asia, and Western Pacific.
In the Americas, there were 6,186,805 suspected cases of dengue reported in the first 15 weeks of 2024. To put this into perspective, according to the Pan American Health Organization (PAHO), this figure represents an increase of 254% compared to the same period in 2023. Of these cases 5,928 were confirmed and classified as severe dengue.
Europe and the U.S. Battle Measles – Again
Initially, doctors in the Tuzla Canton of the Federation of Bosnia and Herzegovina thought the rash on young Imran’s* stomach could be scarlet fever. Or maybe it was Kawasaki disease. As reported by Eurosurveillance, that was in early December 2023. By Christmas, four of Imran’s preschool classmates had been admitted to the hospital with measles. By mid-January 2024, another epidemiologically linked case – again originally misdiagnosed as the much less contagious scarlet fever – presented in a neighboring canton. Two more quickly followed. Between the last week of December and the middle of February, the Balkan nation had reported 141 new measles cases.
Barts Health Trust’s Dr. David Harrington said the misdiagnoses should not be unexpected.
“Many front-line clinicians won’t have seen measles for several years,” he told Medscape UK. “So good education and training and collaboration between public health and infection specialists with those in primary and emergency care is key.”
The Economics of Resistance
It would be extremely difficult to calculate, with any high degree of accuracy, the global economic impact of insecticide resistance. For starters, we must consider that insect management plays a pivotal role in a variety of sectors – agriculture, home and garden, forestry, structural applications, and vector control. Analysis of the totality of economic impacts arising from resistance in any one of these sectors quickly becomes a complicated interplay of variables that interact within that given system.
To account for the full economic impact, one must layer in the amount being spent on insect management and how much of that investment is lost to resistance, but also the economic impact of losses to the overarching objectives of a given program.
To calculate the impact, you must first calculate what is at risk.